In the world of chronic skin conditions, psoriasis is fairly common. It’s estimated to affect up to 8.5% of people worldwide, and over 7.5 million in the United States. (1,2)
For most people, it’s annoying and frustrating because it flares up without notice. It might get better from time to time but never completely goes away…and there is no cure.
Medications are available to help control it, but most of them come with undesirable side effects, especially with long-term use. Here’s another thing:
Many people aren’t aware that psoriasis increases your risk of some other health problems.
If you’ve been diagnosed with, or think you might have this skin condition, it’s important to learn more about the causes, and the lifestyle changes you can make to help manage it.
Not only will they improve your symptoms, but also, they’ll reduce your risk of developing other related health problems.
What Does Psoriasis Look Like?
Psoriasis is a type of skin rash that’s frequently confused with eczema, because they look similar, and both cause itching and discomfort. The main difference is that it tends to have a more thick, scaly, gray or silver appearance.
Also, the itching you experience is usually not as intense as eczema but your skin can be painful, sting or burn. Unlike eczema, psoriasis can also affect your nails, and it may cause painful joints in some people.
There are several different types of psoriasis and they all look different: (3)
Plaque psoriasis
Almost 90% of diagnosed cases suffer from this type. It often appears on the scalp, knees, elbows, lower back, face, hands and feet. Plaque psoriasis usually has raised, red patches along with a buildup of silvery-gray or white dead skin cells. It also has defined edges, and might look like a large scab.
Guttate psoriasis
This form of the skin rash condition affects about 10% of cases. Some people have this type only, and others have it along with plaque rashes. Guttate looks like small, individual red spots that are not usually as thick or raised as plaque psoriasis. The spots can number in the hundreds and usually appear across the stomach, back or limbs. One big trigger tends to be strep infections.
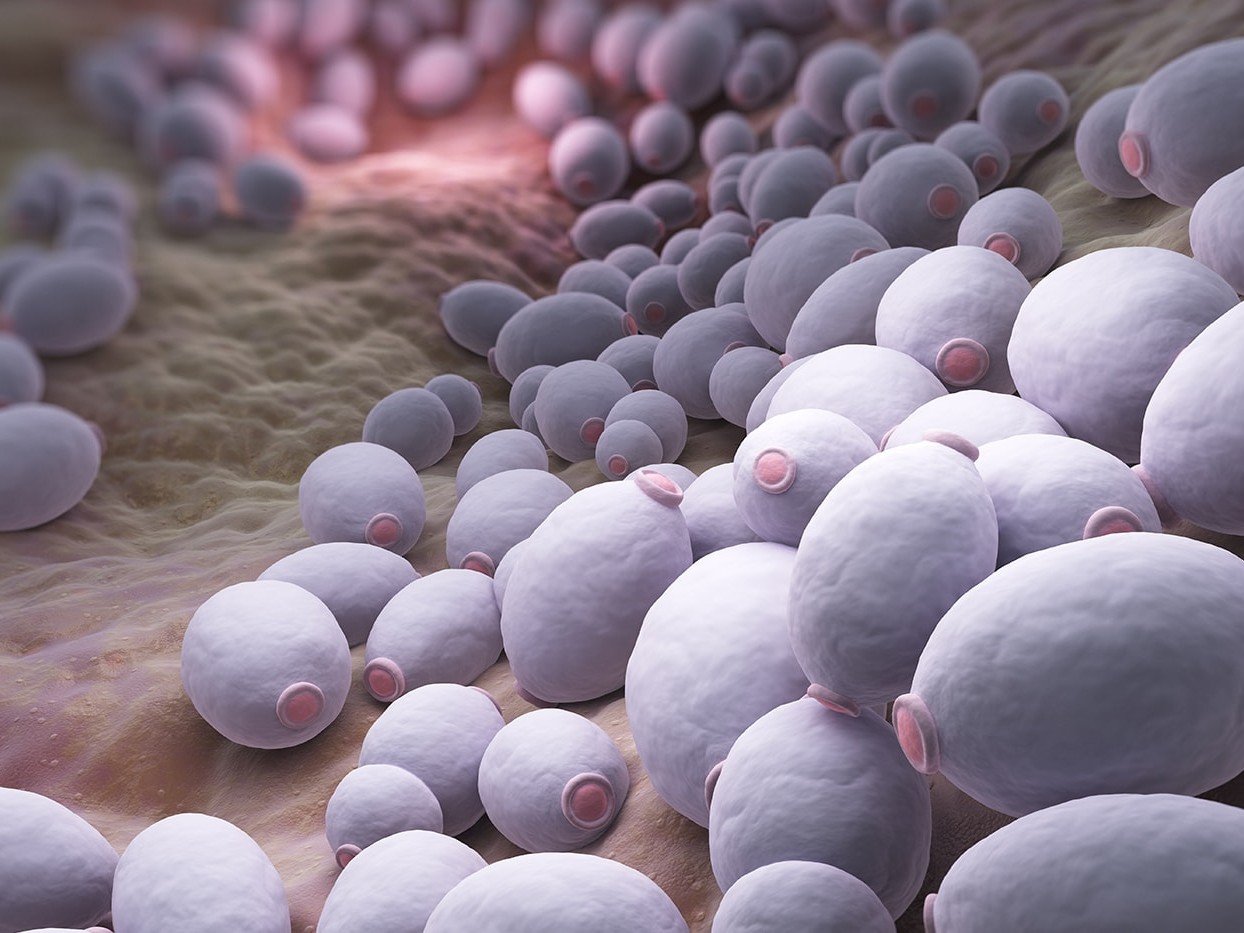
Inverse psoriasis
Inverse psoriasis looks like large areas of red, shiny, smooth lesions. It shows up in the folds of your body, especially the armpits, groin, and under the breasts. Inverse psoriasis is more common if you’re overweight and have deep skinfolds. Most people with this type also have other types of psoriasis, and candida or fungal overgrowth can be a trigger.
Pustular psoriasis
Pustular psoriasis has white blisters surrounded by red skin, and it usually appears on the hands and feet, but in more serious cases, it can cover large sections of your body. Pustular psoriasis runs in cycles. First, the skin reddens, then the blisters appear, and finally, the blisters dry and become scaly.
Erythrodermic psoriasis
Erythrodermic psoriasis is the rarest, but also the most serious form of psoriasis. It only affects about 3% of those with psoriasis, but it requires immediate medical treatment if it occurs. It’s characterized by an extremely red rash that looks like a bad sunburn. It’s often accompanied by severe pain and itching, and the skin can peel in sheets.
The Causes And Triggers of Psoriasis
Psoriasis is a hereditary disease, but researchers have noticed that only about one third of those who are diagnosed with psoriasis have other family members with it. (3) The rest have no family history at all.
It’s also an autoimmune disease, so whether you have the genes or not, psoriasis happens because your immune system starts attacking your healthy skin cells. It doesn’t kill them, but an inflammatory response to something causes them to multiply and grow much faster than they should.
Instead of taking about 23 days for your skin cells to mature, die and slough off, they mature in as short as 3-5 days. (4) They also change form and texture, and the result is those thick, scaly patches.
The job of your immune system is to fight off invaders like viruses, bacteria or other toxins, and keep you healthy. Occasionally, however, the system goes haywire, and gets hyper-activated.
In an autoimmune disease like psoriasis, your immune system starts running on “auto-pilot”. Instead of destroying the bad bugs, it starts attacking your healthy cells by mistake.
Autoimmune diseases are often genetic, but they don’t always act up unless something sets them off.
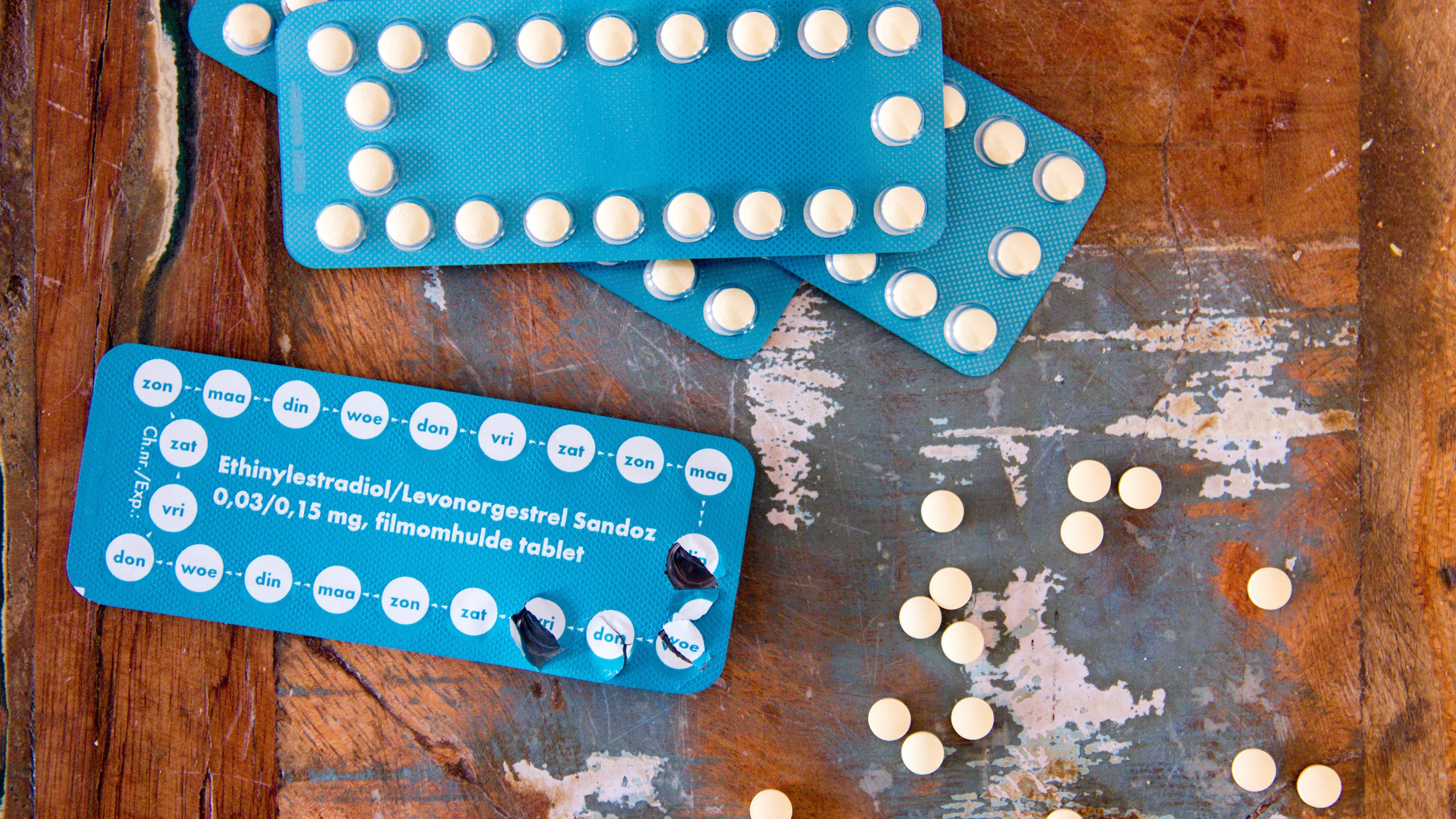
Psoriasis can be triggered by an illness or infection (strep throat is often what causes guttate psoriasis), a poor diet, excess weight gain, certain medications, chronic stress, excessive and frequent alcohol use, a bad sunburn or environmental toxins, like pollution or cigarette smoke. (3, 4,5)
Other triggers can include gut dysfunction, as well as gut microbiome imbalances (including H. pylori infections).
It’s important to know that psoriasis is not contagious, so you can’t catch it or pass it on to anyone else.
Diagnosing Psoriasis
In most cases, your dermatologist can diagnose the different types of psoriasis just by examining your skin. If he or she needs a closer look, they can also do a skin biopsy. Examining the skin’s cells under a microscope will confirm psoriasis if they appear thickened and inflamed.
Psoriasis can also impact your nails and your tongue. Geographic tongue is one potential red flag for psoriasis.
Because psoriasis is both hereditary and an autoimmune disease, your dermatologist should ask about your family history, as well as your own health history.
If you have blood relatives with psoriasis or other autoimmune diseases, you’re more likely to get it. Having other autoimmune diseases yourself, or having had a recent illness, or major life stressor are also triggers for psoriasis.
Discovering that you have an autoimmune disease means that you need to begin looking at your health puzzle from a root cause approach. This means looking at other systems of your body beyond your skin, such as your digestive system and liver.
Looking for tests you can do? Here’s an excellent list.
Health Conditions Related To Psoriasis
As if having painful, scaly patches on your skin isn’t enough for you to endure, you should also be aware that psoriasis is linked to several other health conditions.
Psoriatic arthritis affects up to 40% of psoriasis suffers, usually around 7-10 years after you’re diagnosed. (5) It causes swelling and pain in the joints, and symptoms can range from mild to severe. Most people who develop psoriatic arthritis have signs of the condition in their nails, so make sure your doctor checks them.
Uveitis is an inflammatory disease that affects your eyes and causes blurry vision. Psoriatic conditions slightly up your chances of developing this eye disease. (3) Have your eyes checked regularly, and tell your eye doctor you have psoriasis.
Depression is also common among those with psoriasis and is estimated to affect 46% of this population. (2) The disease can make you self-conscious, and it’s stressful to deal with, which impacts your quality of life. One study found that 16.5% of people who deal with psoriasis suffer from major depression. (7)
Heart disease. It’s hard to imagine that a skin rash could be related to your heart, but it’s true. People with psoriatic issues tend to be at as much as 58% higher risk for a heart attack. (3)
Researchers aren’t quite sure why, but it could be that this skin rash condition (or medications for it) is also linked to obesity, insulin resistance (also known as prediabetes), and high cholesterol levels. (5,6) These things all increase the risk of heart disease, so it’s important to clean up your diet, lose weight if necessary, and do all you can to keep your heart healthy.
Other autoimmune diseases. For some reason, autoimmune diseases like to travel in groups. If you have one, you have a higher risk of developing others, (8) and it’s no different with psoriasis.
Other common autoimmune diseases to be on the watch for include celiac disease, Hashimoto’s, rheumatoid arthritis, Crohn’s disease and lupus. Be aware that there are nearly 100 known autoimmune diseases, so listen to your body in case another one is starting to act up.
Medications And Lifestyle Treatments For Psoriasis
There is no cure for psoriasis, but there are successful treatments available. (1,3,4)
Many people respond well to phototherapy, a UV light or laser treatment, which can slow the growth of skin cells and reduce inflammation so your skin can heal. Dermatologists may also prescribe topical creams like corticosteroids, vitamin D, or retinoid cream (a form of vitamin A) to help slow the growth of skin cells, decrease the scaling, and reduce the redness.
There are also systemic medications that work inside the body to suppress the immune system. Biologics and newer medications are more targeted. They work by quieting only the part of your immune system that is causing your psoriasis.
Each of these treatments has its pros and cons, so make sure you talk to your doctor about the medication’s track record and any side effects, especially if you need to use it long term.
In addition to conventional treatments, it’s wise to work on supporting the overall health of your body and your immune system.
That involves cleaning any junk foods or processed foods out of your diet, and adopting an anti-inflammatory diet that’s rich in fruits, vegetables and healthy fats from nuts, seeds and avocados.
For some, nightshade vegetables can be an issue.
Many people find a gluten and dairy free diet to help their symptoms, and reduce the risk of developing other autoimmune diseases.
Eating better not only reduces inflammation throughout your body, but also, it improves your blood sugar, cholesterol, weight, and even your mood – so your risk of those related health problems will also be minimized.
This all said, it’s important to not go overboard in eliminating too many foods from your diet. Elimination diets like AIP are not meant for long term use and can contribute to food fear and nutrient depletion.
If you are stuck on a limited elimination diet or aren’t getting results, it’s best to get help!
Finally, talk to a clinical nutritionist about using supplements, especially vitamin D, probiotics and prebiotics, and omega-3 from fish oil. They can support a healthy immune system and reduce inflammation.
Ultimately getting a root cause approach evaluation is invaluable because that will ultimately tell you what type of supplementation would be best for you!
And don’t forget to address your stress. Everyone has it, but if yours is especially bad, it may be triggering a worse case of psoriasis.
Explore meditation, yoga, or talk therapy to alleviate any symptoms of stress, anxiety or depression. Studies have found that minimizing stress tends to improve symptoms as well as the way you manage your disease. (9)
1) Psoriasis resource center. American Academy of Dermatology. https://www.aad.org/public/diseases/scaly-skin/psoriasis. Accessed September 24, 2018.
2) Møller AH, Erntoft S, Vinding GR, Jemec GB. A systematic literature review to compare quality of life in psoriasis with other chronic diseases using EQ-5D-derived utility values. Patient related outcome measures. 2015;6:167
3) About psoriasis. National Psoriasis Foundation. https://www.psoriasis.org/about-psoriasis. Accessed September 24, 2018.
4) Habashy, J. Psoriasis. Medscape. March 27, 2018. https://emedicine.medscape.com/article/1943419-overview. Accessed September 24, 2018.
5) Kimball AB, Gladman D, Gelfand JM, Gordon K, Horn EJ, Korman NJ, Korver G, Krueger GG, Strober BE, Lebwohl MG, Foundation NP. National Psoriasis Foundation clinical consensus on psoriasis comorbidities and recommendations for screening. Journal of the American Academy of Dermatology. 2008 Jun 1;58(6):1031-42.
6) Owczarczyk-Saczonek AB, Nowicki RJ. Prevalence of cardiovascular disease risk factors, and metabolic syndrome and its components in patients with psoriasis aged 30 to 49 years. Advances in Dermatology and Allergology/Postȩpy Dermatologii i Alergologii. 2015 Aug;32(4):290.
7) Cohen BE, Martires KJ, Ho RS. Psoriasis and the risk of depression in the US population: National Health and Nutrition Examination Survey 2009-2012. JAMA dermatology. 2016 Jan 1;152(1):73-9.
8) Ali FR, Warren RB. Psoriasis and susceptibility to other autoimmune diseases: an outline for the clinician. Expert review of clinical immunology. 2013 Feb 1;9(2):99-101.
9) Rousset L, Halioua B. Stress and psoriasis. International journal of dermatology. 2018 May 4.