Lichen Sclerosus is a chronic skin condition that affects six times as many women as men. (1) It’s most commonly diagnosed in postmenopausal women, between the ages of 40 and 60. (1)
Lichen sclerosus causes changes in the skin that result in areas that look white, thin, and wrinkled. It may appear on various parts of the body, but it’s most often seen in the external genital and/or anal areas.
When it is on your private parts, it tends to cause intense itching with irritation to the perianal area that can range from embarrassingly uncomfortable to downright miserable.
There is a slight increased risk of cancer associated with this condition, so it’s important to have it diagnosed and treated early. (1,2)
The Most Common Symptoms Of Lichen Sclerosus
Visible signs of lichen sclerosus include patches on the skin that are shiny, white and wrinkled, like tissue or parchment paper. Cracks, fissures or blisters may appear, and there may also be purplish patches or red areas. (1,2,3)
Extragenital lichen sclerosus can appear on any part of the body, especially on the bends of the wrist, the upper torso, around the breasts, on the neck, or in the armpits.
In very rare cases, lesions may appear in the mouth.
Aside from cosmetic aspect, lichen sclerosus on the body usually doesn’t have any other symptoms, other than some possible itching.
The condition is far more common in the genital area though.
In women, it appears around the vulva and/or anus.
It’s not anywhere near as common for men to develop this skin condition, but in most cases, it appears on the foreskin of the penis in uncircumcised males. (3)
If lichen sclerosus progresses in these areas, the inflammation it causes can lead to the growth of significant and permanent scar tissue. This may result in genital deformities that cause urinary or sexual dysfunction.
The most common symptom of genital lichen sclerosus is itching. It can be bothersome and intense enough to keep you up at night, affect normal daily activities, and put a damper on your sex life.
Scratching the affected areas may cause tears in the skin, which can sting and burn, especially with urination. Scratching also makes the affected areas more susceptible to bacteria and infections.
Possible Causes of Lichen Sclerosus
Estimates vary, but lichen sclerosus is thought to affect as many as 1 in 30 postmenopausal women. (4) Even though it seems like a fairly common condition, not much is known about what causes it.
Medical experts do know that it’s NOT a sexually transmitted disease, and it’s not contagious in any way.
Here’s what they suspect may be causes of lichen sclerosus: (1,2,3)
It may be an autoimmune disease. Autoimmune diseases are often triggered by a perfect storm of dietary, environmental, and physical factors.
When they come together, your body goes into overdrive. Instead of fighting off the bad guys, it mistakenly attacks healthy tissues or organs.
Autoimmune diseases also like to travel together, so someone who has one, often has others. People (especially women) with lichen sclerosus are also more likely to have other autoimmune diseases like psoriasis, alopecia, vitiligo, or Hashimoto’s hypothyroid. (5,6)
It may be in your genes. Studies suggest a genetic link because about 12% of women with the condition report having a family member with it too. (6)
Fluctuating estrogen levels likely play a role.
Because the condition is most common among postmenopausal women, researchers believe a drop in estrogen levels may be a trigger. (6)
In uncircumcised men, it’s thought that the enclosed, moist area under the foreskin may promote the condition. (5)
Diagnosing Lichen Sclerosus
Lichen sclerosus can be diagnosed by a dermatologist, gynecologist, or general practitioner. In more advanced cases, this is usually done with just an examination of the affected area.
For extragenital cases, or in very early cases of genital lichen sclerosus, the signs may not be as clear, so your doctor might biopsy a small area of the skin to confirm a diagnosis and rule out other similar skin conditions.
The problem for many people, is that it’s frequently self-diagnosed as a chronic yeast infection because of the genital itching.
It’s also often misdiagnosed, or worse – it’s not diagnosed at all because it can be embarrassing to discuss.
It’s important to know that it won’t go away with over the counter antifungal treatments. And, even though it may not cause significant symptoms for some people, it can get worse for anyone who has it.
Advanced cases of lichen sclerosus can cause permanent scarring along with structural and functional deformities in the anal/genital areas.
In addition, there appears to be a slightly increased (about 5%) risk of developing a type of skin cancer known as squamous cell cancer of the vulva or penis (2,3) – so if you suspect something, get checked.
Looking for tests you can do? Here’s an excellent list.
Treating Lichen Sclerosus
Like other chronic skin conditions, there is no cure for lichen sclerosus in adults (however, it does usually go away in young children). If it’s diagnosed early though, it can be treated and managed so it won’t bother you or develop into a bigger problem.
Medications that your doctor may prescribe include a strong topical corticosteroid cream or injection, (3) or immune-suppressing medications that reduce inflammation on the skin.
Low-dose ultraviolet light therapy may also be an option for certain cases. Most people experience relief from the itching within a few days or weeks, and repair of the affected skin within a few months.
Unfortunately, the medications will not repair any areas that are damaged due to scarring.
In addition to treating the condition itself, it’s important to explore and fix the root cause.
While many people have a genetic predisposition toward lichen sclerosus or other autoimmune diseases, something must trigger them.
In the case of lichen sclerosus, that may be a reaction to an environmental trigger (i.e. a personal hygiene product that you’re reacting to), chronic stress (which weakens your immune system), or a diet that promotes inflammation and leaky gut.
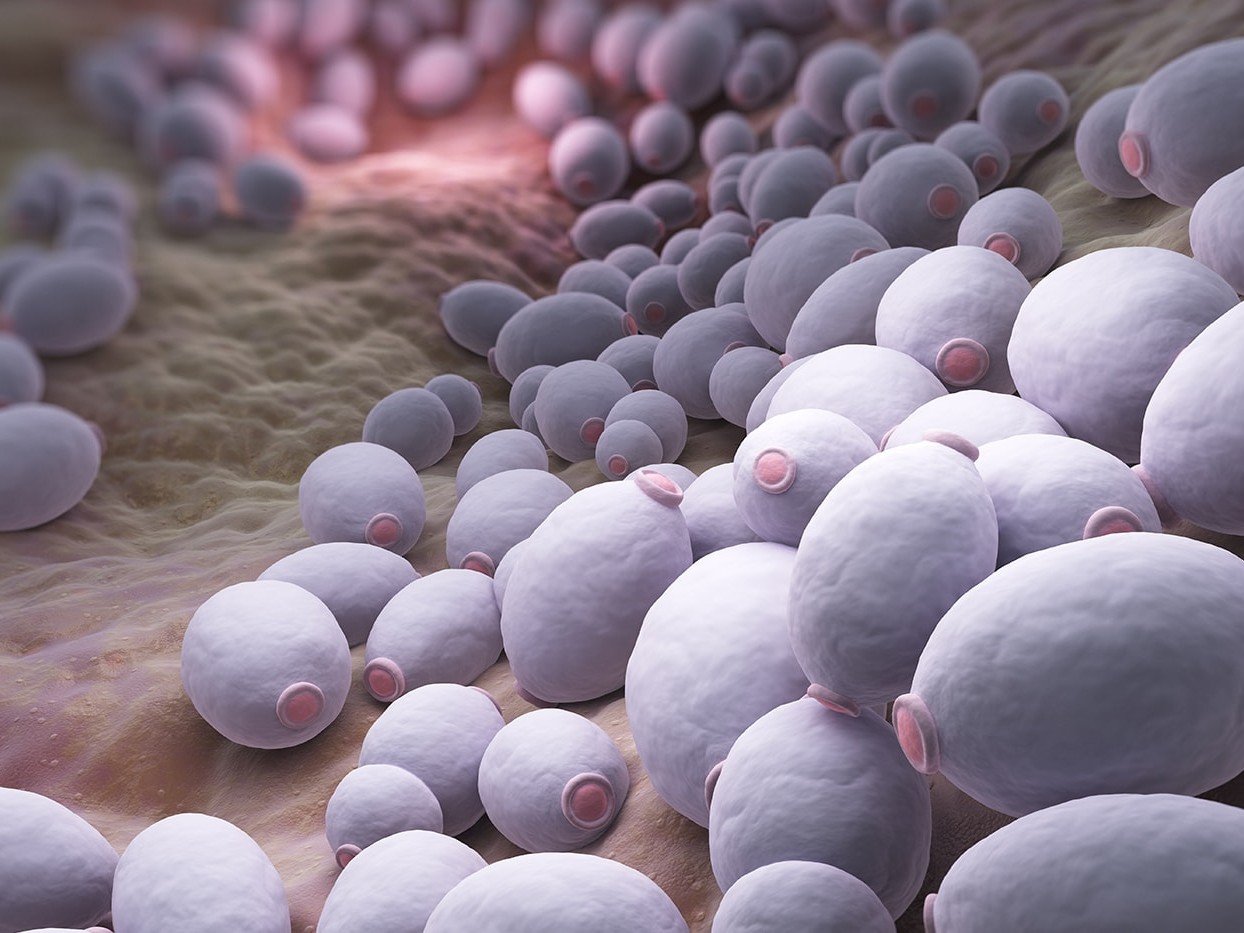
It’s not surprising to see an overgrowth of candida and possibly other unfriendly gut bugs show up in your GI tract, which only adds to the problem.
It’s always worth it to keep a symptom journal to help identify any potential triggers.
Note if any soaps, lotions, laundry detergents and even toilet paper seem to make your symptoms worse.
Also, tune into your emotions – do your symptoms flare up or did they start when you were under increased stress?
Finally, work with a nutritionist to examine your diet.
It’s unclear if there’s a direct diet link to this condition, but your diet certainly impacts your entire immune system – including the immune system in your gut.
Those good bacteria influence all aspects of your health. Interestingly, many skin conditions are associated with a less than ideal microbiome.
Eating more fruits, vegetables, probiotic-rich foods and healthy fats helps to feed those healthy bacteria and reduce inflammation in your body.
On the other hand, if you’re eating many processed foods, refined carbohydrates, or foods that your gut doesn’t like, those may be making your condition worse.
There isn’t a specific diet for lichen sclerosus, but there is some thought that a low oxalate diet may be helpful.
Oxalate or oxalic acid, is a naturally occurring organic compound found in some plant foods.
It’s excreted in the urine, and those with high levels of oxalic acid in their urine may find that eliminating high oxalate foods helps to minimize the inflammation and pain associated with lichen sclerosus. Foods that are especially high in oxalic acid include: (7)
- leafy greens, especially spinach, kale, Swiss chard, and collards
- okra
- potatoes (both white and sweet)
- rhubarb
- blackberries
- raspberries
- tangerines
- dried figs and apricots
- wheat bran; whole wheat bread; wheat germ
- nuts and nut butters
- chocolate
- dark beer
- most forms of soy
Also, keep in mind that fungal overgrowth can contribute to high levels of oxalic acid in the urine. As mentioned before, you should investigate whether Candida or other fungal organisms are playing a role.
You're Not Alone
Lichen sclerosus can be an uncomfortable condition to live with, and embarrassing to discuss.
You can rest assured though, you’re not alone with it, and help is available.
Talk to your doctor about medications, and surround yourself with a good healthcare team to work on your triggers.
This is a very manageable condition that does not have to impact your quality of life.
1) Lichen sclerosus. National Organization for Rare Disorders. https://rarediseases.org/rare-diseases/lichen-sclerosus/ . Accessed November 27, 2018.
2) Lichen sclerosus in females. British Association of Dermatologists. http://www.bad.org.uk/shared/get-file.ashx?id=291&itemtype=document. Accessed November 27, 2018.
3) Pappas-Taffer, L.K., Lichen sclerosus. Medscape. May 17, 2018. https://emedicine.medscape.com/article/1123316-overview. Accessed November 27, 2018.
4) Wedel N, Johnson L. Vulvar lichen sclerosus: Diagnosis and management. The Journal for Nurse Practitioners. 2014 Jan 1;10(1):42-8.
5) Fistarol SK, Itin PH. Diagnosis and treatment of lichen sclerosus. American journal of clinical dermatology. 2013 Feb 1;14(1):27-47.
6) Sherman V, McPherson T, Baldo M, Salim A, Gao XH, Wojnarowska F. The high rate of familial lichen sclerosus suggests a genetic contribution: an observational cohort study. Journal of the European Academy of Dermatology and Venereology. 2010 Sep;24(9):1031-4.
7) Low oxalate diet. University of Pittsburgh Medical Center. https://www.upmc.com/-/media/upmc/patients-visitors/education/unique-pdfs/low-oxalate-diet.pdf. Accessed November 28, 2018.