Vitiligo is an autoimmune skin condition that causes your skin to lose its color in certain areas.
It affects an estimated 0.5 -1% of the world’s population. (1) About half of those who have it, first notice it in their twenties, and most will have it for the rest of their lives. (2)
Although it rarely causes any health problems, vitiligo’s effects are more than just cosmetic.
Most people who deal with vitiligo also struggle with social anxiety, embarrassment, or other emotional problems because of the change in your appearance. Some may also have health problems due to autoimmune diseases that are related to vitiligo.
Here’s what you should know about vitiligo and how to manage it.
The Signs and Symptoms of Vitiligo
Vitiligo begins as small light or white-colored patches on the skin. The patches result from a loss of melanin, the pigment that gives skin its color.
Vitiligo is a progressive disease. But if the loss of pigment is very slow, you may go for years without seeing any change in the patches. (2)
When the condition advances, the loss of pigment becomes more noticeable, with large irregular-shaped white patches either in one localized area or on many parts of the body.
Unfortunately, there isn’t a way to determine how fast or slow the loss of color in your skin will happen. Some people report that they notice more pigment loss if they undergo periods of emotional or physical stress. (3)
Vitiligo is most noticeable on people who have darker skin, but it can affect anyone of any skin color. It often starts on the hands, wrists, fingertips, feet, or around the mouth or eyes.
Although it’s less common, you can also lose the pigment in your hair, eyelashes, eyebrows, inside of your mouth or on your genitals.
The areas of your skin that are affected can sunburn easier, or sting when you’re exposed to sunlight. Some people have pain or itching in the affected areas, especially at the beginning stages of pigment loss.
Research also suggests that vitiligo can affect cells in the inner ear and eye, which may lead to problems with hearing, eyesight or tear production in a small percent of the population. (4,5)
There are 2 main types of vitiligo, and each looks a little bit different (2)
Non-segmental vitiligo is the most common type. The pigment loss occurs on both sides of the body, such as both hands, feet, legs, etc. It tends to start and stop, but the areas of pigment loss eventually become more noticeable and they expand and cover more of the body.
Segmental vitiligo is less common, and accounts for only about 10% of vitiligo cases. (1) It usually starts earlier in life, affects only one segment (i.e. one hand, foot, leg) of the body, and occurs for about a year, but then stops. In addition, about half of those with segmental vitiligo have some loss of color on the hair on their head, eyebrow, or eyelashes.
The (Suspected) Causes of Vitiligo
The exact cause of vitiligo is still unknown.
The non-segmental type may be caused by damage to the melanocytes (the cells that produce the melanin pigment) from skin trauma or oxidative damage at the cellular level.
Many experts believe that the more common segmental vitiligo is an autoimmune disease with a genetic link. (1,2) About 20% of those with vitiligo also have a close family member with it. (3)
In addition, 15-20% of people with vitiligo have at least one other autoimmune disease like psoriasis, systemic lupus erythematosus, autoimmune thyroid disease, celiac disease, or alopecia areata. (1,4)
Researchers have identified several variations (which are kind of like typos) in genes that regulate inflammation and the immune system’s function on melanocytes. (1)
People who have these genetic “typos” have a greater risk of developing vitiligo. Most of the time your body can still read the instructions on the gene, so it knows how to produce the melanin pigment and protect the melanocytes from damage that happens from inside or outside of the body.
However, in some people, the right combination of environmental triggers, physical or mental stress, an overstressed immune system, and a genetic predisposition, can trigger the autoimmune disease. When that happens, instead of protecting the healthy cells, the immune system attacks healthy melanocytes, and zaps their melanin-making power.
No one knows exactly what triggers vitiligo, but the following things, either alone or in combination, are thought to play a role: (3,5)
- Exposure to certain chemicals
- A bad sunburn or other trauma to the skin
- A virus, infection, or other physical illness
- Emotional stress or a recent stressful personal or family event (5)
- A family history of vitiligo
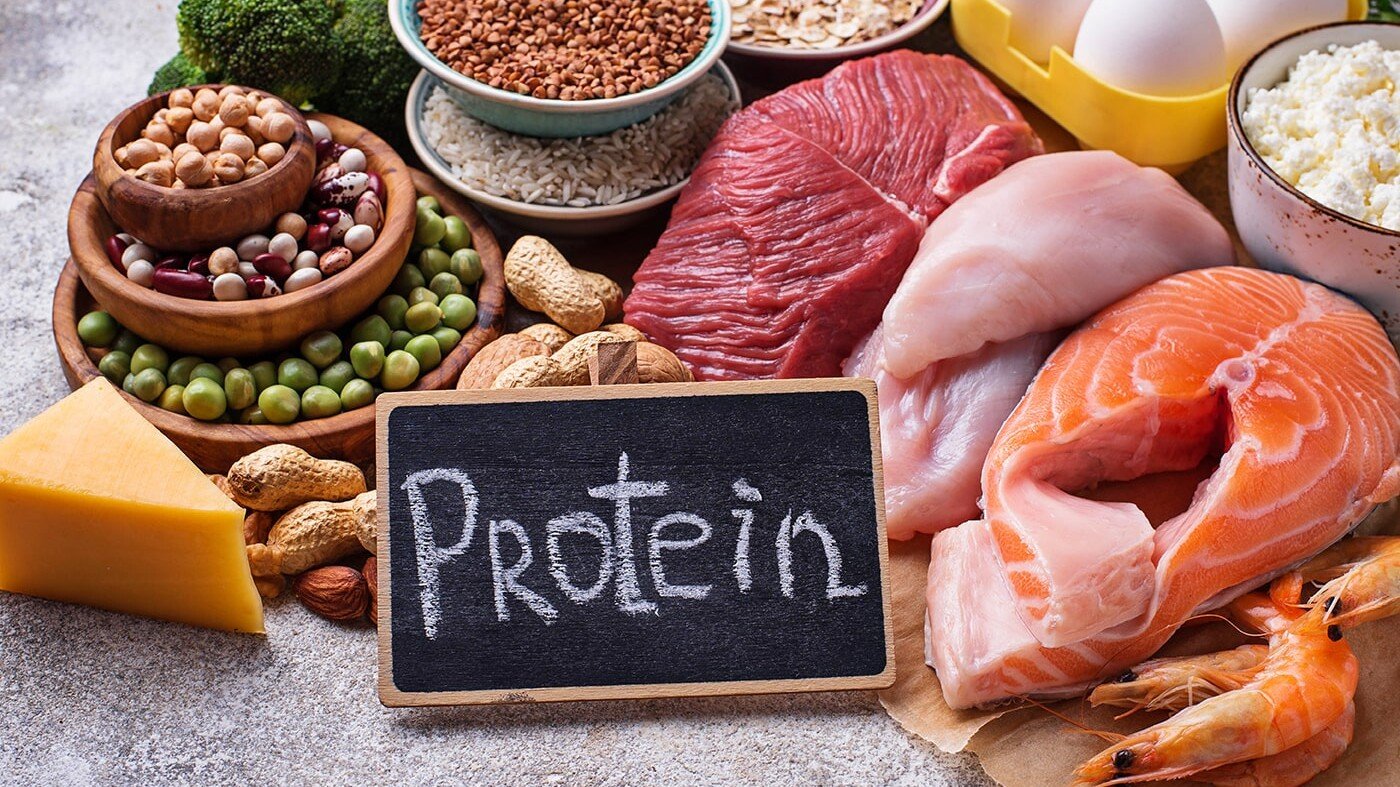
- A weakened immune system due to poor diet or nutrient deficiency
Diagnosing Vitiligo
A dermatologist can diagnose vitiligo by examining your skin and reviewing your medical history. He or she will also ask about your family history, and discuss whether you’ve had any of the possible triggers listed above, or if you’re significantly sensitivity to sunlight. (2)
Vitiligo may be harder to see if you have fair skin. Your dermatologist can use a special light called a Wood’s lamp to highlight any pigment changes.
Because of the suspected autoimmune connection, your doctor may also test for the presence of other autoimmune diseases, especially Hashimoto’s hypothyroid which is more common among those with vitiligo. (2,3,4)
If you’re diagnosed with vitiligo, you should also see an eye and ear specialist to make sure you don’t have problems with eyesight, tear production or hearing problems as a complication of the condition.
Looking for tests you can do? Here’s an excellent list.
Controlling and Treating Vitiligo
Currently, there is no cure for vitiligo.
However, there are medical treatments that can help restore the pigment and color to your skin. They work better on some parts of your body than others. Your best chance of successful treatment is possible the earlier you start upon first noticing pigment changes.
The following are the most common medical treatments for vitiligo: (2,3,4)
Topical corticosteroids are usually the first line of treatment (though they do have potential issues). They suppress the immune system so the melanocytes can begin to make pigment again.
Corticosteroids may take 4-6 months to work, but about 45% of patients have good results, especially on their body or face. The hands and feet are harder to treat.
Lightbox therapy for large areas, or excimer laser treatments for small areas, can also restore pigment. These work best on the face or body, rather than the feet or hands.
About 70% of people with vitiligo notice the color return to their skin with excimer laser treatment, but many treatments are needed, and the downside is that the pigment may fade after a while.
PUVA, or Psoralen plus UVA light is another very effective treatment. Psoralen is a topical or oral drug that makes your skin more sensitive to ultraviolet light. PUVA can be up to 75% effective in restoring melanin to more parts of the body, but as with the other treatments, it doesn’t work well on the hands or feet.
Two less frequently used treatments are surgery and depigmentation. Surgery to transplant areas of skin with color in areas that have lost pigment is an option for adults with stable vitiligo that doesn’t respond to other treatments. However, it comes with the risk of scarring or a patchwork appearance.
Depigmentation is another option for those who have very widespread vitiligo, but it’s considered a last resort for most people. Rather than restoring color to your skin, depigmentation uses medications to kill off any remaining melanocytes, so that all the skin is white.
In addition to traditional medical treatments, it can be helpful to consider complementary treatments in the management of vitiligo.
There are reports of emotional stress as a trigger, (5) so if you’re going through a stressful event like the death of a loved one, divorce, or financial difficulties – or if your vitiligo itself causes significant stress, seek out a good mind-body therapist.
Mind-body interventions like meditation, yoga, and breathing exercises can help with stress management and there is evidence that they can reduce inflammation and enhance immune function, (6) which might slow the spread of vitiligo.
It’s also helpful to work with an integrative nutritionist. They can check for any nutrient imbalances that contribute to a dysfunctional immune system, or dietary intolerances, which might cause autoimmune diseases to flare up.
Those with vitiligo may be low in vitamin D, or have inadequate levels of zinc and copper. (3,7) In addition, some people are unknowingly sensitive to gluten, and have had improvements in their vitiligo and other autoimmune diseases when following a gluten free diet. (7)
Although there isn’t any diet or any one natural treatment that can reverse vitiligo, there are foods, supplements, herbal remedies and probiotics that can help balance your body, support a healthier immune system, and possibly make traditional medical treatments work better.
You’ll have the best results if you work with a medical team to learn about all your options and choose the treatments that work best for you.
1) Vitiligo. National Institutes of Health Genetics Home Reference. https://ghr.nlm.nih.gov/condition/vitiligo#resources. Published December 18, 2018. Accessed December 28, 2018.
2) Vitiligo. American Academy of Dermatology. https://www.aad.org/public/diseases/color-problems/vitiligo. Accessed December 28, 2018.
3) What is vitiligo? Vitiligo Support International. https://www.vitiligosupport.org/treatments_and_research/. Accessed December 28, 2018.
4) Iannella G, Greco A, Didona D, Didona B, Granata G, Manno A, Pasquariello B, Magliulo G. Vitiligo: pathogenesis, clinical variants and treatment approaches. Autoimmunity reviews. 2016 Apr 1;15(4):335-43.
5) Silverberg JI, Silverberg NB. Vitiligo disease triggers: psychological stressors preceding the onset of disease. Cutis. 2015 May;95(5):255-62.
6) Bower JE, Irwin MR. Mind–body therapies and control of inflammatory biology: a descriptive review. Brain, Behavior, and Immunity. 2016 Jan 1;51:1-1.
7)Smith MK, Mohammad TF, Hamzavi IH. Assessment of Dietary Supplementation in the Treatment of Vitiligo. The Open Dermatology Journal. 2017 Feb 28;11(1).