How To Identify And Manage Rosacea
You’re too old for teenage acne and haven’t been out in the sun, right?
That red, acne-like rash that doesn’t seem to clear up may be rosacea. It’s a very common but chronic skin condition that affects up to 16 million people in the U.S. (1)
Rosacea affects both women and men.
Most who develop rosacea are between the ages of 30 and 50. Just like other skin conditions, having rosacea can cause you to worry about your appearance, and it can have a huge impact on your self-confidence.
Don’t let rosacea affect your quality of life. There are ways to manage it, so you can put your best face forward.
What Are The Symptoms Of Rosacea?
The most common symptom of rosacea is redness in the face that looks like blushing or a sunburn. There are four different forms, or subtypes, of rosacea though, and each has different symptoms. (2)
To make matters even more confusing, the symptoms can look different from one person to another. It’s also possible to have more than one subtype at a time. Here’s a bit about each:
Erythematotelangiectatic Rosacea (ETR)
A major, tell-tale sign of ETR is areas of tiny, broken blood vessels on the face, especially on the cheeks, nose and chin. From a distance, those with ETR appear to have a flushed or sun-burned face, but close-up, you can notice large areas of broken blood vessels that look like spider veins. It’s common for skin to be sensitive, flush easily, burn or sting. It can also be dry and rough.
Papulopustular Rosacea (PPR)
PPR causes red areas with acne-like breakouts and oily skin. Sometimes the skin can be swollen or have raised plaques. It’s often sensitive, and may sting or burn. PPR can also have can also have areas of broken blood vessels.

Rhinophyma
This subtype is a rare form of rosacea that causes the skin, especially on the nose, to thicken and become bumpy with visibly broken blood vessels and large pores. It mainly affects men over the age of 40. (3) Rhinophyma often starts as one of the other subtypes.
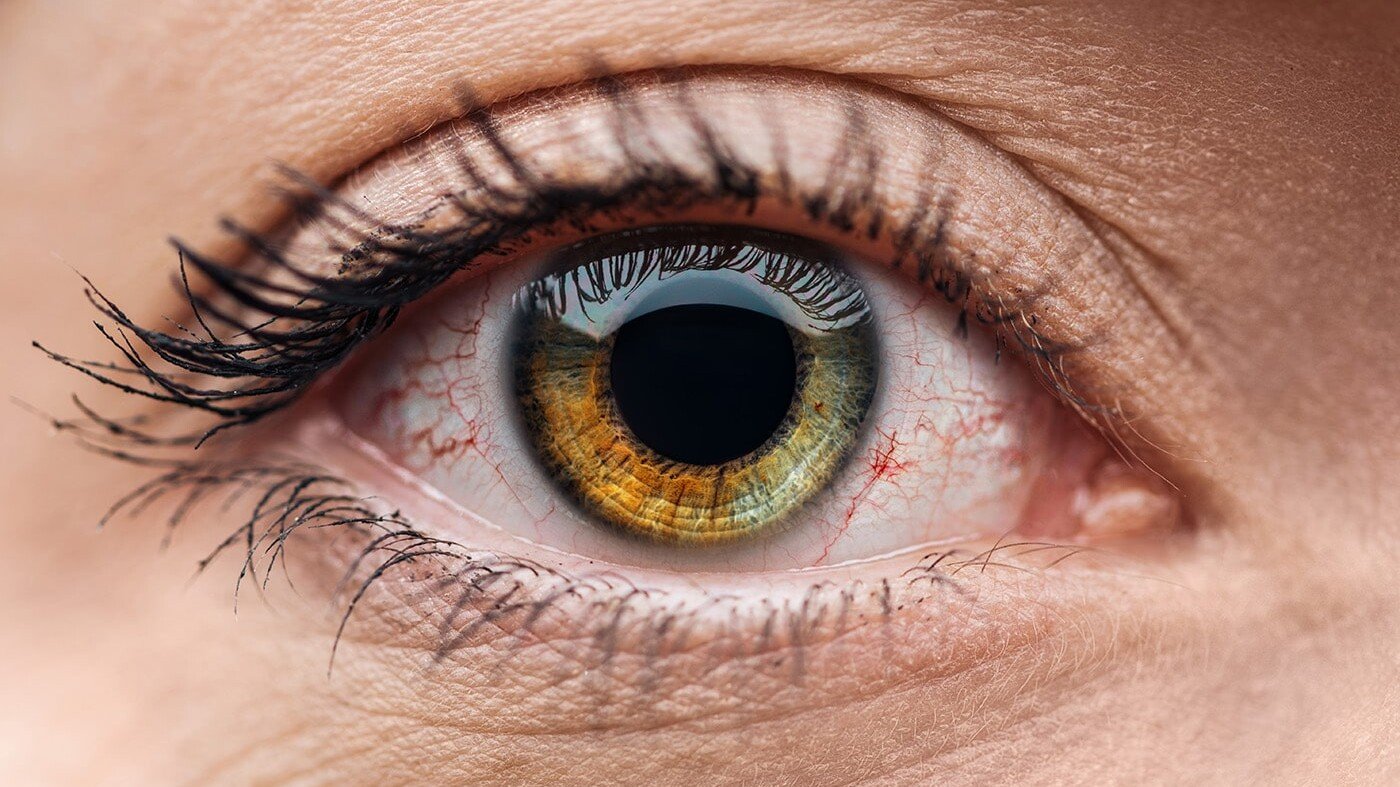
Ocular Rosacea
About 50% of those with rosacea have this type that affects their eyes. (1) Ocular rosacea causes itchy and irritated eyes that are watery, and appear red or bloodshot. It can also cause cysts to form on the eyelids, and it may cause your eyes to be sensitive to light or even result in blurry vision.
What Causes Rosacea?
Although anyone can develop rosacea, it seems to run in families, so researchers believe there is a genetic component. It also affects more fair-skinned people who blush or flush easily.
People with or who have had more severe acne in the past (especially cystic acne) are at increased risk of developing rosacea. (1)
The exact cause of rosacea isn’t clear, but there are a LOT of surprising triggers.
The bacteria H. pylori, which can live in your digestive tract and cause ulcers, is commonly found in people with rosacea.
It appears that H. pylori might increase risk, or play some role in triggering the skin condition, but it’s not a guarantee. (1,3) Either way, it’s important to look at supporting your oral microbiome since this type of infection can actually start in your mouth.
SIBO (short for Small Intestine Bacterial Overgrowth) can certainly be a trigger that’s often overlooked.
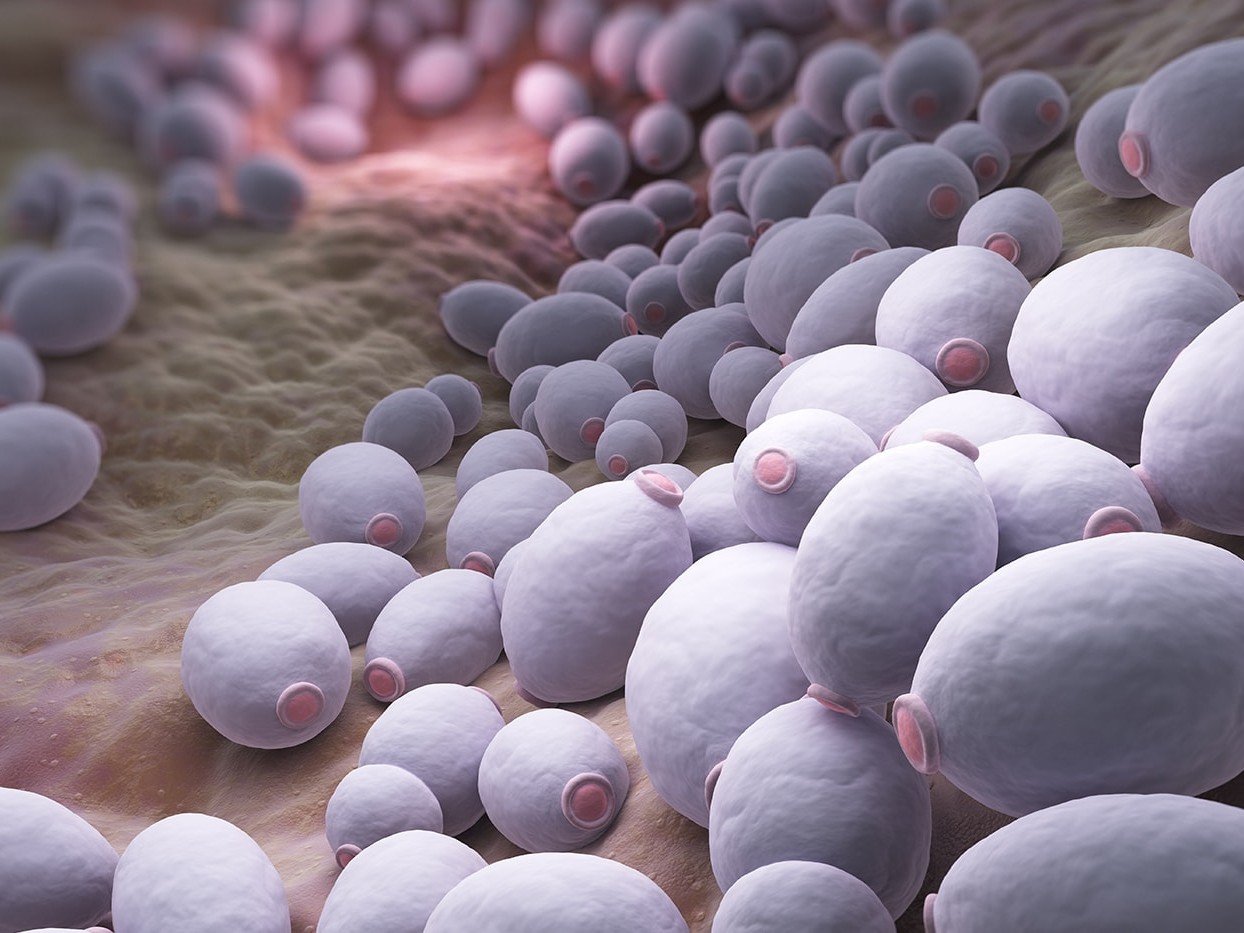
Candida overgrowth is another gut trigger that may be underlying the rosacea. You’d want to confirm be cautious of trying a Candida Cleanse if you suspect you have Candida because they can often make skin issues worse from my clinical experience.
A malfunction in the skin’s immune system might trigger an inflammatory reaction that leads to rosacea. Usually, your skin’s immune system is programmed to detect and repair damage from things like sun exposure or microbes, but in those with rosacea, that innate immune system doesn’t appear to work correctly. (2)
Tiny mites might play a role. It sounds like something out of a sci-fi film, but everyone’s skin is home to microscopic Demodex folliculorum mites. They live off skin cells, and rarely cause any problems.
Occasionally, however, they get out of control and multiply too quickly. It’s unclear if the mites are a cause, or if they multiply in response to whatever triggers rosacea.
Either way, researchers have noticed that those with the skin condition also have more of these mites. (1,2,3)
Your diet might be triggering rosacea. If you notice your rosacea gets worse periodically, think back to what you recently ate or drank.
Common dietary triggers include alcohol, caffeine, hot (as in temperature) foods or beverages, and spicy foods. Other foods that have been reported to trigger rosacea include citrus fruits, certain vegetables, chocolate, cheese, and yogurt (4,5).
In addition to specific food triggers, scientists believe there may be a link between your gut microbiome (the healthy bacteria) and rosacea.
They’ve noticed that there’s a higher incidence of rosacea among people with Crohn’s disease, ulcerative colitis, celiac, and small intestine bacterial overgrowth (SIBO). (6)
These gastrointestinal conditions are linked to a microbiome that’s not as well-fed as it should be. Adding more prebiotic and probiotic-rich foods can make a huge difference in your rosacea, since your microbiome controls much of your immune system.
It might be temperature-related. Anything that increases your body temperature, or just makes you feel uncomfortably warm can also be a trigger.
This might include hot flashes associated with menopause, intense exercise, saunas, steam or hot baths, sun, and even emotional stress that gets you “hot under the collar”. (5)
Sometimes you can just blame it on the weather. Hot, cold, sun, wind, and humidity are all reported triggers. (5)
Finally, it might be related to something you’re using on your skin. Check with your dermatologist to see if your lotion or makeup contains an ingredient that might be making things worse.
How Is Rosacea Diagnosed?
Rosacea is often confused with other skin conditions like acne or dermatitis. A dermatologist can accurately diagnose rosacea by examining your skin and asking about your symptoms and medical history.
There is no lab test that can confirm a diagnosis. When your doctor examines your skin, he or she will look for one or more of the following signs to confirm rosacea and identify the subtype: (3)
- Transient flushing
- Redness that does not go away
- Red pimple-like bumps (papules)
- Red bumps with pus (pustules)
- Tiny spider-like blood vessels
- Eye problems, including redness or cysts
Looking for tests you can do? Here’s an excellent list.
What Types Of Treatments Can Help With Rosacea?
You might be inclined to skip the doctor and just put up with your symptoms if they’re mild.
However, you should know that rosacea can get worse, and it may cause damage to your eyes if you develop ocular rosacea.
The good news is, there are many treatments, depending on the subtype you have, and most are effective at minimizing and controlling the symptoms.
Laser or intense pulsed light (IPL) treatments are effective at removing blood vessels on the face.
Topical antibacterial, antifungal, or retinoid treatments are often used for mild PPR.
In more advanced cases, oral systemic treatments may be needed.
Treatment for ocular rosacea usually includes carefully washing the eyelids and applying metronidazole gel.
Complementary treatments are an important part of managing rosacea.
Diet and lifestyle changes may prevent symptoms from progressing, and they can help minimize the use of stronger medications.
If you’re not doing it already, keep a journal and track your symptoms along with potential triggers like diet, temperature, stress or anything else that seems relevant.
Talk to a clinical nutritionist who can look deeper and help you identify the root causes underlying your rosacea. And they can give you guidance on whether it is worth doing an elimination diet or using any supplements.
Cutting out triggers, and working to strengthen the army of healthy bacteria in your gut can make a world of difference both in your rosacea and your overall immune system.
1) All about rosacea. National Rosacea Society. https://www.rosacea.org/patients/allaboutrosacea.php. Accessed October 8, 2018.
2) Rosacea. American Academy of Dermatology. https://www.aad.org/public/diseases/acne-and-rosacea/rosacea#overview. Accessed October 8, 2018.
3) Clark, C., Rosacea causes and treatments. Pharmaceutical Journal online. https://www.pharmaceutical-journal.com/files/rps-pjonline/pdf/CPDonline_1-4.pdf. Accessed October 8, 2018.
4) Weiss E, Katta R. Diet and rosacea: the role of dietary change in the management of rosacea. Dermatology practical & conceptual. 2017 Oct;7(4):31.
5) Factors that may trigger rosacea flare-ups. National Rosacea Society. https://www.rosacea.org/patients/materials/triggers.php. Accessed October 8, 2018.
6) Katta R, Kramer MJ. Skin and diet: An update on the role of dietary change as a treatment strategy for skin disease. Skin Therapy Lett. 2018 Jan;23(1):1-5.