Got dandruff? If so, you’re not alone. About half of the world’s population, and at least 50 million Americans (1) have it too. But if your itching and flaking doesn’t improve with dandruff shampoo, or if it spreads to your eyebrows, face, or other parts of your body, it might be a more serious skin condition known as seborrheic dermatitis.
Seborrheic Dermatitis is the bigger, tougher cousin to dandruff. Living with it can be embarrassing and impact your quality of life.
While there is no cure for seborrheic dermatitis, there are ways to tame and manage it, so you can coexist peacefully and even wear your favorite black sweater again.
What Are The Symptoms Of Seborrheic Dermatitis?
Like so many other chronic skin conditions, seborrheic dermatitis is a relapsing condition, which means it can come and go without notice. It’s similar to dandruff, in that it often causes flaking on your scalp.
However, its symptoms are more severe, and unlike dandruff, it doesn’t improve as you get older – in fact, it can get worse. (1)
With seborrheic dermatitis you may have thickened, crusty or scaly patches on your scalp or onto your hairline. It may also appear on your eyebrows, around the sides of your nose, in your ears, or on your upper chest or back.
The skin in these areas may also be red and itchy. Seborrheic dermatitis occurs in oily areas of the skin, where there are more sebaceous or oil-secreting glands. (2,3)
A form of seborrheic dermatitis, commonly known as cradle cap, affects many infants. It causes scaly patches on a baby’s scalp, or on the eyelids or nose, but it clears up within a few months and usually disappears completely by age 1 (2).
The other, chronic form of seborrheic dermatitis is less common. It affects between 1-3% of healthy adolescents and adults, but most people tend to be between the ages of 30 and 60 (1,2).
In certain segments of the population, especially those with a compromised immune system, the prevalence can be much higher. (2,3) When you develop seborrheic dermatitis as an adult, it’s considered to be a lifelong condition.
What Causes Seborrheic Dermatitis?
Just like eczema, psoriasis, or other chronic skin conditions, the exact cause of seborrheic dermatitis isn’t known. However, you can rest assured that it’s not caused by poor hygiene and it’s not contagious, so you can’t pass it on to someone else. Although it can be uncomfortable, embarrassing, and affect your self-esteem, seborrheic dermatitis isn’t harmful to your body in any way.
More than likely, there are several factors that come together to trigger this skin condition.
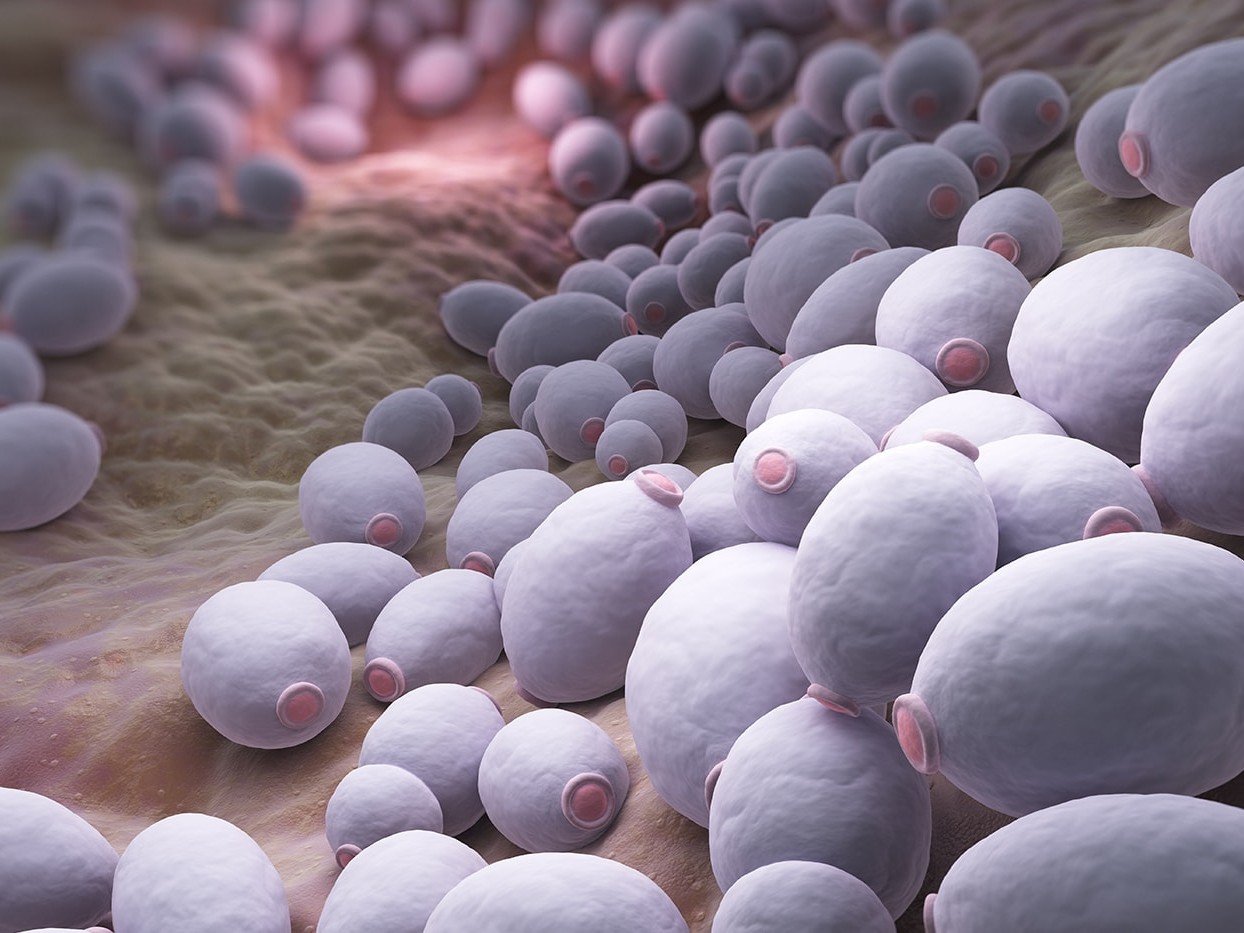
Most researchers agree that seborrheic dermatitis is related to a fungal yeast, known as Malassezia, (1) that lives in oily areas on the skin. In some people, Malassezia disrupts and invades the skin’s outer layer. This causes an inflammatory response that results in seborrheic dermatitis.
Interestingly, the same yeast is also found in people with normal, healthy skin. That suggests there’s something else that triggers the inflammation.
Whether the inflammatory response is due to something inside or outside of your body isn’t completely clear. Here’s what researchers have noticed about seborrheic dermatitis and those who develop it: (1,4)
- It affects slightly more men than women
- It may be hereditary, but that’s not a guarantee that you’ll get it
- Your risk increases as you get older, possibly because your skin isn’t as great at fighting off pathogens.
- The weather may play a role. For many, it flares up when it’s cold and dry outside.
- People often report it’s triggered by stress, anxiety or depression.
- Those with neurological conditions like Parkinson’s disease, traumatic brain injury, epilepsy, spinal cord injury, or those recovering from a stroke are at increased risk.
- It’s more prevalent in immune-compromised individuals, especially those with HIV or AIDS, lymphoma, or organ transplant recipients. It’s estimated that between 34-83% of those with a compromised immune system have seborrheic dermatitis. (5)
- It may be triggered by certain medications, especially interferon, lithium, or psoralen
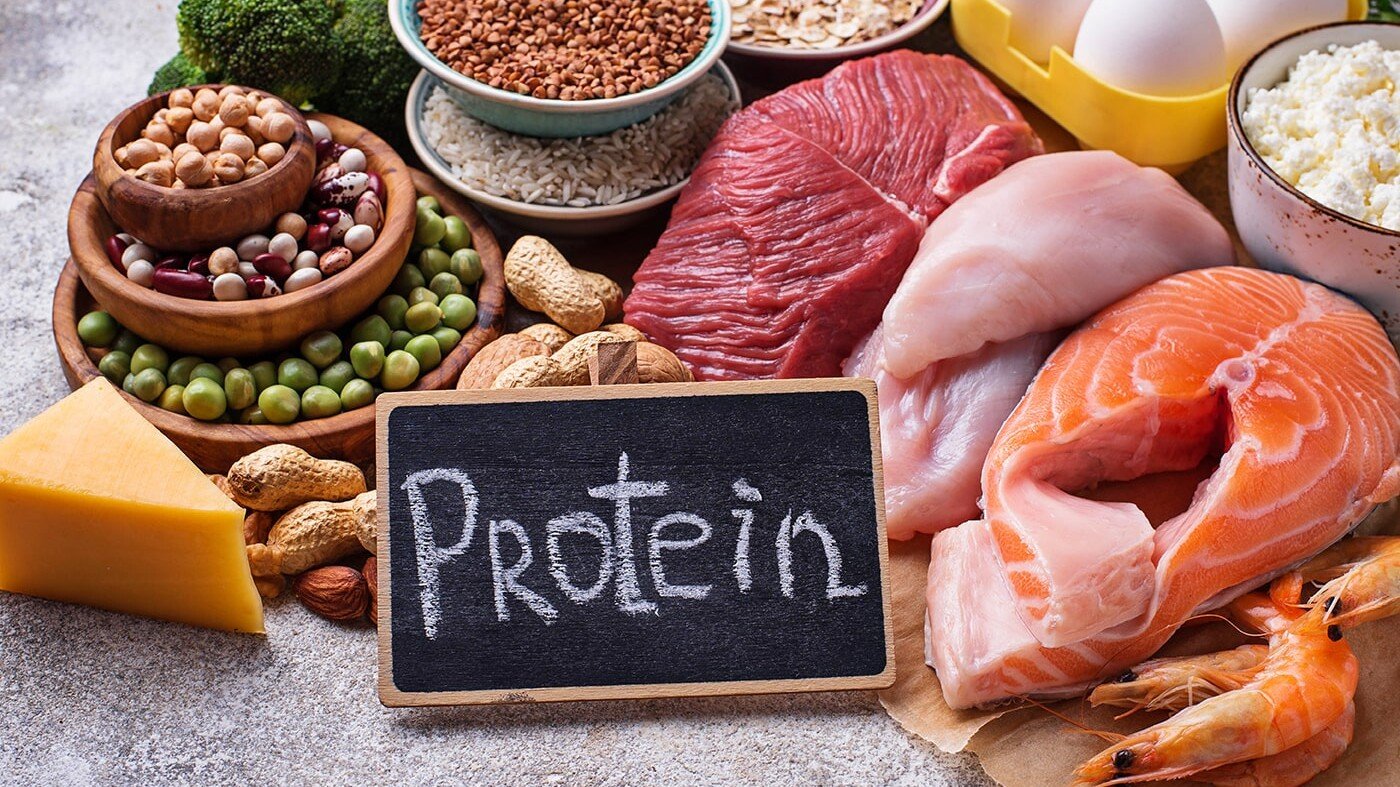
- Your diet may play a role. One study found that women who ate a “western diet” (full of fast foods, processed foods and too much sugar) had a 47% increased risk of developing seborrheic dermatitis. (6) It’s also more common among those with eating disorders.
How It’s Diagnosed
Because it can resemble other skin conditions like eczema, psoriasis, or even systemic lupus, it’s best to get an accurate diagnosis from a dermatologist. Each of these conditions requires a different treatment, so the first step is knowing what you’re dealing with.
In most cases, a dermatologist can diagnose seborrheic dermatitis just by examining the areas of your skin that are affected and reviewing your symptoms and health history. In some rare cases, a skin biopsy may be necessary to rule out other, more serious skin conditions.
Looking for tests you can do? Here’s an excellent list.
Treating Seborrheic Dermatitis
It’s a lifelong, chronic condition, so it’s important to say on top of seborrheic dermatitis. The good news is that doing so can manage it and help prevent a relapse.
Over-the-counter dandruff shampoos containing selenium sulfide, coal tar, or zinc pyrithione may work well to reduce scalp flaking. Tea tree oil can also decrease symptoms.
For longer-term control, your dermatologist will probably recommend using an antifungal shampoo to control the yeast on your scalp. Using this once a week, and leaving it on your hair for at least 5 minutes has been shown to prevent a relapse of the scalp symptoms. (5)
The most effective treatments for your face and body include antifungal creams and topical corticosteroids.
In addition to traditional medical treatments, there can be a connection with overgrowth of Candida Albicans and other fungal organisms in your gut. That said, “Candida Cleanses” and “Candida Detoxes” tend to make things worse (not better).
It’s best to get guidance on the best way to support rebalancing your gut if Candida is at the root of your seborrheic dermatitis.
And of course, make sure you clean up your diet as much as possible. Eating a more whole foods diet and moving away from processed foods can help your skin and boost your immune system so you can fight inflammation better.
An anti-inflammatory diet that includes fruits and vegetables with each meal, along with fish, nuts, seeds and legumes is especially beneficial.
Although research is mixed, some people have noticed improvements in their symptoms from supplements like biotin, probiotics and Aloe Vera.
Some essential oils, especially borage, evening primrose, and black currant seed oil may also reduce symptoms. Talk to your nutritionist to learn more about these.
You might also find it helpful to keep a journal to identify your triggers. While you can’t change your age, sex or genes, you can take steps to reduce your stress, strengthen your immune system, avoid cold climates, or minimize any other triggers you might identify.
While seborrheic dermatitis hasn’t been linked to allergies, there may be certain soaps, detergents, or foods that you react to, and you’ll likely feel better if you eliminate them.
Living with seborrheic dermatitis can be stressful, but managing it doesn’t have to be. Start by talking to your doctor and other health professionals. Together, you can put a plan in place to get it under control and keep it there.
1) Borda LJ, Wikramanayake TC. Seborrheic dermatitis and dandruff: a comprehensive review. Journal of clinical and investigative dermatology. 2015 Dec;3(2).
2) Seborrheic dermatitis. American Academy of Dermatology. https://www.aad.org/public/diseases/scaly-skin/seborrheic-dermatitis#overview. Accessed October 29, 2018.
3) Seborrheic dermatitis. National Eczema Association. https://nationaleczema.org/eczema/types-of-eczema/seborrheic-dermatitis/. Accessed October 29, 2018.
4) Sanders MG, Pardo LM, Franco OH, Ginger RS, Nijsten T. Prevalence and determinants of seborrhoeic dermatitis in a middle‐aged and elderly population: the Rotterdam Study. British Journal of Dermatology. 2018 Jan;178(1):148-53.
5) Clark GW, Pope SM, Jaboori KA. Diagnosis and treatment of seborrheic dermatitis. American family physician. 2015 Feb 1;91(3).
6) Sanders MG, Pardo LM, Ginger RS, Kiefte-de Jong JC, Nijsten T. Association between diet and seborrheic dermatitis: a cross-sectional study. The Journal of investigative dermatology. 2018 Aug 18.